Metabolic and bariatric surgery
More than half of all metabolic bariatric procedures are performed in women in the reproductive age group
Metabolic and bariatric surgery often improves fertility in women resulting in more spontaneous or planned conception after surgery
- Weight loss reduces obesity related pregnancy risk such as HPT in pregnancy, gestational diabetes and issues with labour/delivery
- However pregnancy after bariatric surgery (especially gastric bypass) has an increased risk of micronutrients deficiency
In general it is recommended to postpone pregnancy until weight loss stabilizes, typically 1 year after surgery
- To allow time for maximal weight loss and making positive lifestyle changes
- To reduce the risk for nutritional deficiencies which may have a negative impact on the foetal development and maternal health
Nutrient needs often increase during pregnancy as the foetus grows and maternal blood volume increases
It is important that all patients have an early consult with the obstetrician, GP and dietitian for a tailored individual approach to antenatal blood test and adequate nutritional supplements
| Special mention for pregnant ladies after bariatric surgery Higher doses of folic acid may be needed such as 4-5g a day Iron and vitamin B12 replacement is almost routinely given Calcium and vitamin D supplements >50nmol/L is recommended Caution with vitamin A (retinol) supplement because it may be potentially teratogenic Fetal growth monitoring with ultrasound at 28, 32 and 36 weeks is a minimum Blood tests such as HbA1C is performed instead of OGTT Please note: Regular over the counter vitamin supplements are not likely to be sufficient *Specialised post op bariatric multivitamin supplements are sometimes recommended especially for deficiencies in iron, folate, B12 and vitamin D *Note that high levels of folic acid may also mask vitamin B12 deficiency, which is also important in the foetal neurological development* *Vomiting during pregnancy is associated with thiamine (B1) deficiency *Foods high in vitamin A or retinol based (A) supplements should be avoided in pregnant women to avoid vitamin A toxicity but at the same time vitamin A deficiency should be avoided (Beta carotene is recommended) |
| Polycystic ovarian syndrome Increased BMI is associated with hormonal imbalance, irregular menstrual cycle, low ovulation or anovulation. PCOS rate is reported to be up to 36% of women before surgery and after bariatric surgery there is about 96% improvement. *Bariatric surgery may be beneficial to restore endocrine equilibrium and irregular menstruation. PCOS may affect 5-10% of women in their reproductive age group, characterised by hyperandrogenism, anovulation and multiple cyst in the ovaries. PCOS is one of the leading causes of infertility in women. It is an endocrinological disorder and may be related to or aggravated by obesity with increase production of adipokines (TNF, leptin), decrease sex hormone binding globulin (SHBG) and insulin resistance (hyperinsulineamia leads to increased ovarian androgen secretion). Some studies showed that losing 5% of body weight in the obese PCOS population may help restore ovulatory cycles and spontaneous conception. With adequate weight loss there can be significant improvements in menstrual dysfunction, hirsutism and obesity/PCOS related co-morbidities (HPT, T2DM, dyslipidaemia). Bariatric surgery have been shown to improve the abnormal sex hormone axis by *Decrease in dehydroepiandrosterone, oestradiol and anti Mullerian hormone *Increase in sex hormone binding globulin Bariatric surgery has been shown to reduce gestational DM and pregnancy related HPT. *Reduction in antepartum pregnancy related complications is likely due to weight loss and the metabolic improvements. *Reduction in labour complications such as obstructed labour (higher Caesarean section rates), anal sphincter injury and post partum haemorrhage. There are no standard guidelines but most surgeons and physicians recommend a 12 to 18 months interval after bariatric surgery before conceiving. However please note however *Some studies have shown that a shorter interval time (< 1 year) have similar maternal/perinatal outcomes compare to those who conceive 1 year after bariatric surgery. *Some studies suggest that pregnancy less than 18months post op may have a higher anaemia and Caesarean section rates. |
| Bariatric surgery and pregnancy Younger female patients should sough proper contraceptive advice from their GP or obstetrician after undergoing bariatric surgery. There may be reduced effectiveness of oral contraceptive pills, weight gain side effects of certain hormonal treatment and consideration for the use of implants or intra uterine devices. The Roux Y gastric bypass and some other major bypass procedures may pose a special risk during pregnancy. *GIT symptoms such as abdominal pain/distension and nausea/vomiting is difficult to distinguish between a post op complication and the usual symptoms of pregnancy (morning sickness, hyperemesis gravidarum) *Imaging test such as abdominal CT is contra-indicated. *Bariatric related surgical complications such as small bowel obstruction, internal hernia, intussusception/volvulus may have a disastrous outcome in the maternal and fetal group. Screening for gestational diabetes is important. Obese patients even after successful weight loss surgery still have a higher risk to develop gestational diabetes compare to normal weight individuals. *OGTT may be unreliable and intolerable after bariatric surgery. As a result of bariatric surgery and patient dietary changes, there is the potential for micronutrient deficiency. Pregnancy related nausea and vomiting or food intolerances may exacerbate the issue. Meta analysis shows that vitamin A, B1, B6, B12, C, D, K, iron, calcium, zinc, selenium and phosphorus levels in pregnant women after bariatric surgery may be significantly reduced. *Please note vitamin A has potential teratogenic effects and the levels should be checked and supplementation reduced if necessary. Adequate nutrition, vitamin and mineral supplements is the most crucial from 10 weeks prior to gestation to 14 weeks after gestation, the most crucial period for the embryo development. Clinicians can measure maternal gestational weight gain of the mother, antenatal blood test for micronutrient deficiencies and for fetal birth weight. *It is important to observe for intrauterine fetal growth retardation, small for gestational age and neurological development. There may be a slightly higher risk for preterm labour. |
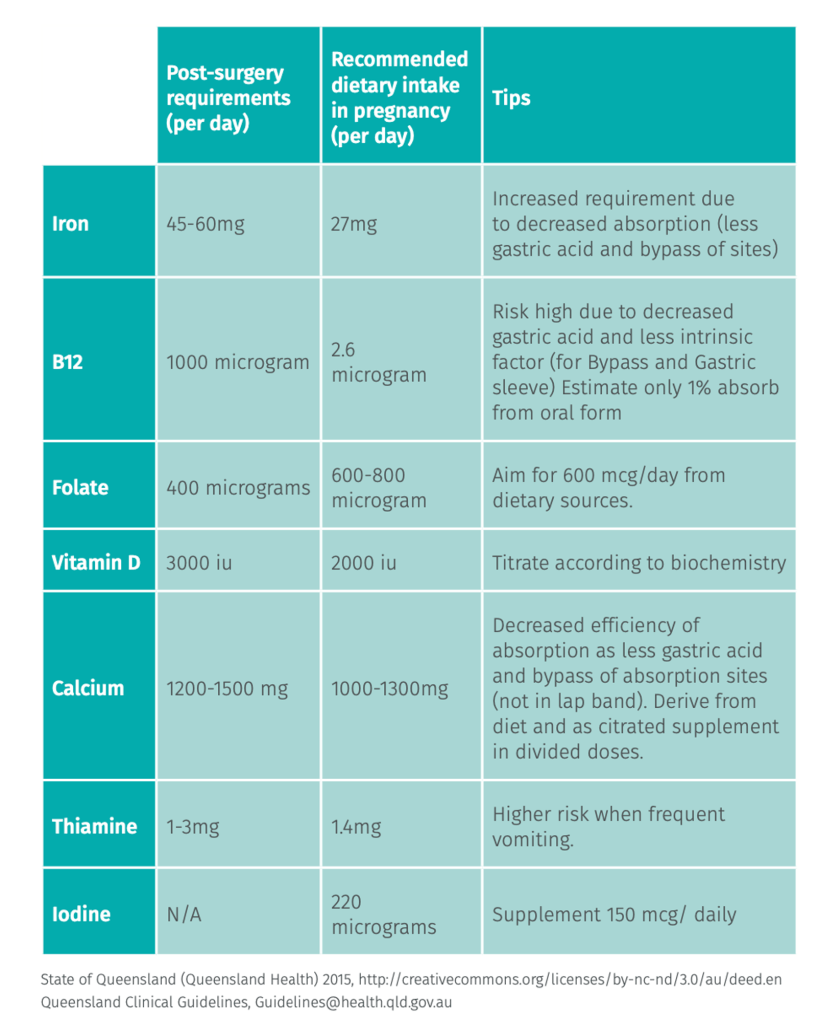
| Nutritional issues Macronutrients during pregnancy During pregnancy the protein demands increases as well The daily recommended protein intake is 46g (0.8mg/kg ideal body weight) during the first trimester and 71g (1.1g/kg) during the second and third trimester After bariatric and metabolic surgery, the protein intake should be about 60g (1.5g/kg ideal body weight) Micronutrient deficiencies to consider: Folate deficiencies can cause neural tube defects, preterm labour and placenta related complications Vitamin B9 and B12 deficiencies are associated with a higher risk for abortion and preterm labour Vitamin B1 deficiency may cause cardiac and neurological complications Vitamin C, E, iron, selenium and zinc deficiency are associated with preterm birth Vitamin A deficiency can lead to intrauterine growth retardation, retinal damage and childhood blindness *But retinol vitamin A is considered teratogenic *Hence the beta carotene form is recommended The normal post bariatric multi vitamin supplements often has retinol Hence a substitute to pregnancy supplements are needed The micronutrient requirements during pregnancy recommendation can vary, usually the daily recommendations are: Folic acid 0.4-1mg Iron 45-60mg Thiamine (B1) >12mg Beta carotene (A) 5000 IU Vitamin E 15mg Zinc 15mg Copper 2mg Selenium 50 micro gram |
| Short summary on deficiencies and consequences Vitamin A visual impairment Vitamin K intra cranial ahemorrhage Vitamin B12 neural developments Vitamin B9 (folate) neural tube defects |