| Reframing metabolic and bariatric surgery (MBS) outcomes By Prof Carel Le Roux, University College Dubin Background infformation: *Obesity is a chronic and relapsing disease with over 200 medical co-morbidities and complications *Apart from weight loss (primary end points) and resolution of Type 2 diabetes and hypertension (secondary end points), obesity doesn’t have any defined treatment targets, limiting our ability to provide effective obesity care *Obesity treatment targets incorporate patient preferences and practical care pathways to improve obesity treatment outcomes *Medications (Semaglutide, Tirzapetide) and metabolic bariatric surgery can achieve 20-25% weight loss New proposed IFSO treatment targets include *BMI <27, improve mechanical outcomes such as joint pain and sleep apnoea *Waist:hip ratio <0.53 to reduce metabolic risk, T2DM or cardio-vascular risk factors This new structured plan may help align clinician and patient target, help track patient progress and integrate obesity into a chronic disease model 5 key themes influencing patient decisions about medication or surgery: *Accessibility (private insurance, other cost, location) *Polypharmacy (better maintenance weight loss outcomes and health improvements, to reduce long term reliance on medication) *Future health fears (mobility, independence) *Support systems (social isolation) *Information mismanagement (better patient insight) Surgeons have to inform the patients about: *Clear weight loss target, other medical and physical goals *Align with patient preferences *Provide practical supportive tools (recommend multi disciplinary care, other treatment strategies as well as metabolic bariatric surgery) Multidisciplinary care typically includes dietitian, exercise physiologist, psychologist (behavioural modification), obesity management medication, GP, physician input and surgery |
| Sleeve vs Roux Y gastric bypass By Dr Paulina Salminen, University of Turku Finland JAMA 2022 Aug 1;157 (8): 656-666. Salminen et al. Effect of laparoscopic sleeve gastrectomy vs Roux-en-Y gastric bypass on weight loss, comorbidities and reflux at 10 years in adult patients with obesity: The SLEEVEPASS randomised clinical trial This is a study from 2008 to 2021 with 10 years follow up from Finland, which reported that *Both Sleeve and RYGBP has substantial weight loss result *RYGBP has 8.4% more excess weight loss (%EWL) at 10 years *Only a small proportion has suboptimal weight loss outcome *There were no statistically significant difference in remission rate for T2DM ***Shorter duration of T2DM pre-op is associated with better resolution rates, highlighting the benefits of early surgical intervention *For HPT the RYGBP has clear advantage for remission rate *There were no statistically significant outcome for OSA and dyslipidaemia between sleeve vs RYGBP 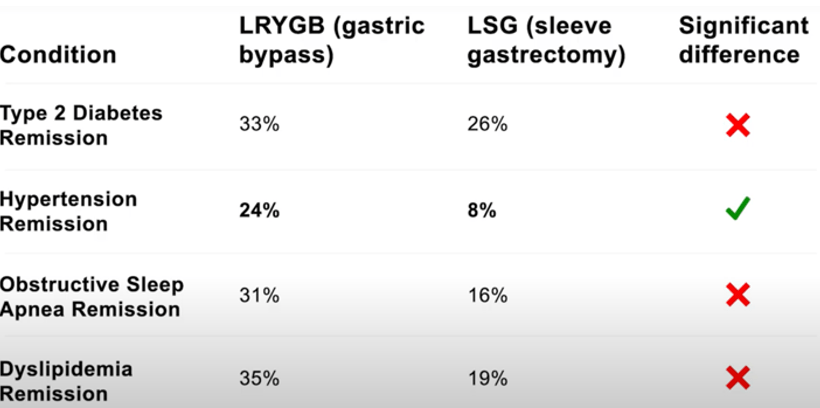 Summary of the study: *Both sleeve and RYGBP are effective for sustained weight loss and has good remission rate for obesity related co-morbiditiies ***Early intervention is critical especially for T2DM *Reflux and oesophagitis more prevalent after sleeve (31%) vs RYGBP (7%) *PPI medications higher in the sleeve vs RYGBP group (61 vs 36%) *Barrett’s oesophagus is equal in both groups at 4% *Sleeve has a higher re-operation rate for reflux *RYGBP has more re-operations for internal hernia *Selection of sleeve vs gastric bypass surgery is dependent on patient preferences, goals in the long term as well as long term follow up, side effects, risk and complications |
| Obesity management medications (OMM) By Dr Ricardo Cohen, Brazil Summary: *Metabolic and bariatric surgery is an effective and safe long term treatment for obesity *GLP-1 RA (Semaglutide, Tirzapetide) has been introduced to be used after surgery for suboptimal weight loss and weight gain recurrence, usually when the weight loss outcome had plateaued *The use of OMM before surgery however has limited evidence at this stage and should be personalized, based on patient or clinician expectation Revision and conversion surgery is technically difficult, has more risk and complications than index operation Emerging therapy such as endoscopic sleeve gastrectomy doesn’t have much long term outcomes, further research is necessary for long term sustainability and safety |
| Safety and efficacy of metabolic bariatric surgery (MBS) By Dr Khaled Gawdat, Egypt Lancet 2021, May 15;397 (10287): 1830-41. Syn, et al. Association of metabolic-bariatric surgery with long term survival in adults with or without diabetes: a one stage meta-analyses of matched cohort and prospective controlled studies with 174 772 participants (1 470 articles) *Table below showing MBS improve life expectancy by 5.1 years (those with no T2DM) and 9.3 years (those with T2DM) *Metabolic bariatric surgery is associated with lower all cause mortality rate and longer life expectancy *The peri-operative death risk was less than 0.1% 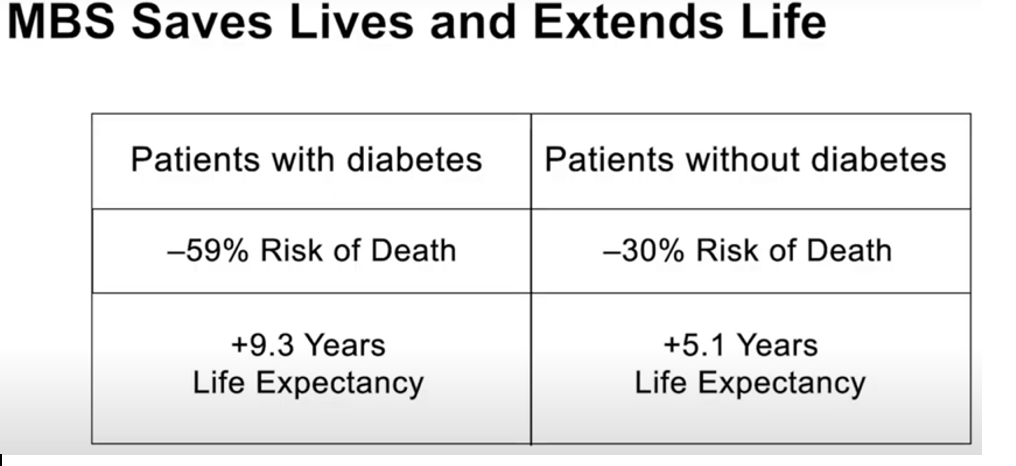 JAMA 2019;322 (13): 1271-1282. Aminian et al. Association of metabolic surgery with major adverse cardiovascular outcomes in patients with Type 2 diabetes and obesity. This is an observational study reported that MBS resulted in *41% lower risk of early death *39% less AMI and strokes https://asmbs.org/news_releases/head-to-head-study-shows-bariatric-surgery-superior-to-glp-1-drugs-for-weight-loss/ 2025 data reported by the ASMBS reported that on average patient reported 24% weight loss 3 years after MBS compare to 5-7% with medications such as GLP-1 RA 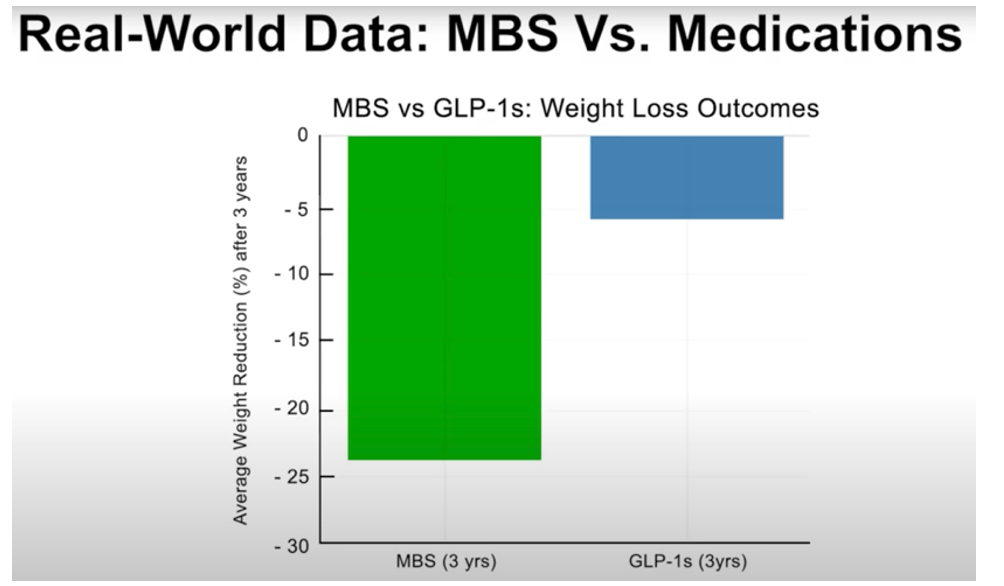 2025 study from Poland concluded that MBS is safe for patients over the age of 65 years provided that proper pre-op assessment is done Similar long term studies in adolescent showed durable weight reduction, remission of T2DM, improvement in quality of life without increased long term complications |
| Multi disciplinary support By Prof Lilian Kow, Australia Structured multi disciplinary support team (GP, physician, surgeon, dietitian, exercise physiologist, psychologist, lifestyle coaches, etc) helps with significant and sustained weight loss result in the long term *Sustained weight reduction 26.5 – 33% over a follow up period of 9 years has been reported with a structured multi disciplinary team *Clinically significant weight loss with 50% showing remission/improvement in T2DM and up to 83% better blood pressure control The integrated care model is for any chronic medical condition *And because obesity is a complex and chronic disease, patients needs a team approach for ongoing care long term care before and after metabolic *With proper support there are improvements in quality of life, physical and mental health (less anxiety and better mood/confidence) |
| Psychological factors By Dr David Sarwer, USA Obesity is often associated with a high burden of psycho-social distress including: *anxiety/depression *eating disorder and substance misuse *interpersonal trauma, PTSD, adverse childhood experience These factors co-exist with obesity, affects treatment adherence, weight loss maintenance, overall well being Patients need to address the psycho-social factors above so that they are prepared for changes after surgery including changes in body image, self esteem, interpersonal social relationship (with spouse, family, work place, etc) Majority of patients undergo significant positive changes in the physical and mental health after surgery But 20-30% of patients may develop negative post-op psychological issues such as *Maladaptive eating behaviour (grazing, binge eating, loss of control) *Body image dissatisfaction *Changes in romantic and social relationship *Depression, suicide (non adherence to dietary plans or post-op care, substance abuse) Pre-op psychologist assessment: *A standard for managing weight loss (for non surgical and surgical patients) *Identify mental health issues or patients factors that may lead to suboptimal outcomes *Educate patients about changes that will be required for the best possible result Post op psychologist intervention: *Treat mental health or behavioural issues after surgery *Address psycho-social aspects and patient’s function in their day to day environment for long term success of metabolic bariatric surgery |
| Obesity stigma By Ximena Salas, Lund University Sweden Surgery can’t remove stigma, the hidden impact of shame and judgement and discrimination (being treated unfairly) people living with obesity faces everyday before or after surgery There exist a general public false assumption that obese patients are lazy, unmotivated, unable to control eating, lacking will power or responsibility to their weight and associated chronic medical disease, non adherence to healthcare recommendations, physical activity and exercises Weight stigma may be: *Perceived (shame, judgement, discirimination from others) *Internalised (turning negative attitudes, stereotypes or prejudice inward towards themselves, leading to self criticism and shame about body dissatisfaction, low self worth) *Anticipated weight stigma (expectation or fear that one will be judged or shame in the future because of their weight by healthcare providers or in social situations) Clinical impacts of weight stigma include *Depression *Anxiety *Chronic stress *Disordered eating *Binge eating *Body dissatisfaction *Lower self esteem and body image issues Women tend to experience weight stigma more intensely Family and community attitude may amplify weight stigma Some patients may choose more risky approaches Weight stigma affects patient weight loss outcome *Some may avoid healthcare intervention *Take extreme measures (medical tourism overseas) *Not disclose the weight loss treatment plan with family or friend or social support Consequences of weight stigma: *Distrust between patient and healthcare providers *Discouraged from seeking medical help *Harm metabolic bariatric surgery recovery and outcomes To manage weight stigma: *Raise patient awareness and education *Encourage family or friends/peers to provide social support *Seek the ongoing care from a psychologist or counsellor |
| The empowerment of motivational interviewing By Violeta Moize, Barcelona University Spain Motivational interviewing is *The patient centred conversation between the patient and healthcare provider, aiming to explore and resolve ambivalence *The healthcare provider listens, to understand the individual reason, values and motivation for change *Motivational interview is not about giving advice or convincing patients to change, it is about working with the patient Motivational interviewing is: *Partnership (working together as equal) *Acceptance (respect without judgement) *Compassion (put patient’s wellbeing first) *Empowerment (help patient find their reasons for change) Motivation interviewing is: *Engaging and building trust *Focusing on health/patient goals and priorities *Evoking to help patient uncover their own motivation, making change that improve their daily lives *Planning together and collaboration The goal is not about weight loss *It is about supporting healthier behaviour, promote greater confidence, better patient satisfaction and healthcare provider experiences *Patient wants to feel more respected, not be judged and becomes more motivated to engage in their care |
| New obesity definition By Prof Francesco Rubino, King College UK Terminology: *BMI has been used for decades as a measure for obesity *Disease is an organ dysfunction with symptoms and signs Now the term clinical obesity is used to define a condition where excess adiposity is directly responsible for impairment of organ function or that the individual is affected by obesity to conduct their daily activities *Clinical obesity management focus on improvement or reversal of organ dysfunction Preclinical obesity is when there is no ongoing impairment of organ function or that the individual is not affected by obesity to conduct their daily activities *Preclinical obesity management focus on risk reduction and prevention of progression to clinical obesity or other related diseases 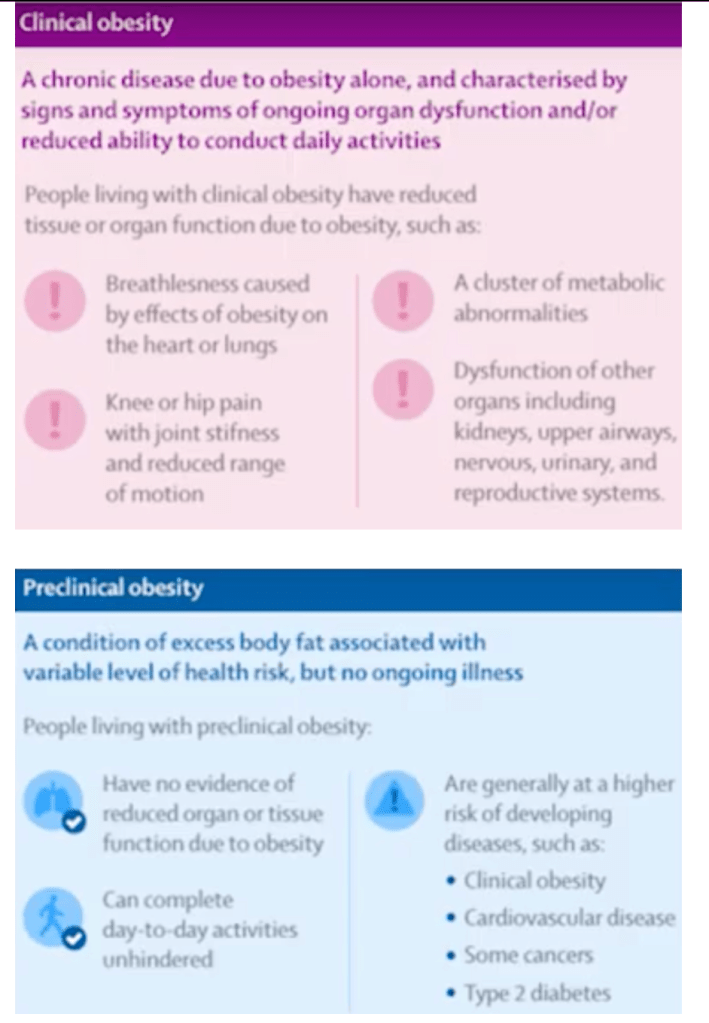 |
| Artificial intelligence By Dr Jaime Ponce, USA AI is transforming medicine and bariatric surgery But the uncertainty remains in: *The reliability of AI in surgical decision making *The ability for AI to improve surgical training *AI improvements in patient care without compromising ethics Current experts consensus states: For surgical training: *AI can objectively evaluate surgical skills, provide personalized feedback and accelerate learning curve for students *Virtual and augmented reality can help trainees improve confidence, reduce operating time, lower complication rate, help identify anatomical landmark *Future surgeons needs AI and robotic training literacy *However concerns remain about the accuracy, reliability and the need for surgeon oversight in complex cases For decision making: *AI can help identify if patient may benefit from surgery and can recommend a standardized procedure ***But evidence showed that the AI model align with expert opinion in only about 30-40% of cases *AI can answer patient enquiries or clinical question with high accuracy in some domain to help reduce cognitive burden ***But risk include over reliance on machines, accountability gaps and diminished critical thinking of the clinician 88% of experts agree that AI can improve efficiency and lower cost of bariatric surgery by optimising process and improving outcomes by integrating electronic health records 80% of experts agree that AI can forecast weight reduction (5 year outcomes), complication risk (VTE risk) and predict re-admissions more accurately than traditional methods and support personalised follow up care AI has to comply with data privacy regulation, with full patient consent Currently the limitations are that: *AI requires large high quality data sets *Has difficulties with the variability in techniques and outcome *There is a lack of transparency *AI has difficulty handling complex visual tasks *Has limited clinician trust *Lack the human element of care (algorithm driven instead) Health care models traditionally has been based on empathy, transparency, prioritise patient education and maintaining doctor-patient relationship In conclusion, AI is not to replace but to support clinicians and to support patients Responsibility, ethics and clinical judgement will still remain in human hands |